Abstract
Background: Acute Myeloid Leukemia (AML) is a disease of older adults, with a median age of 68 years at diagnosis. The NCCN guidelines recommend comprehensive geriatric assessments (GA) be included in clinical practice to guide treatment decisions. Utility of GA in older AML patients in a real-world environment is not yet established. We tested the feasibility of using a modified GA (mGA), administered by patient self-report on a touchscreen computer, real-time use and utility by clinicians and the correlation of mGA results on treatment decision-making.
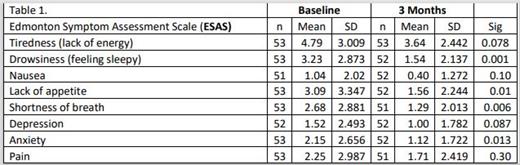
Methods: 77 newly diagnosed patients were recruited from three sites to complete a tablet-based mGA screening at a treatment decision visit. The mGA includes four domains: age, activities of daily living (ADLs), instrumental ADLs, and comorbidities. Survey results along with history of falls was used to create the Frailty Index (FI). Providers were asked what they thought the fit/frailty status of the patient was before viewing the results on a dashboard. After viewing the survey results, the clinician discussed the treatment plan with the patient. Patients received intensive or non-intensive therapy. Additional information was captured on clinical trial enrollment. Baseline and 3 month surveys recorded presence and severity of 8 symptoms using the Edmonton Symptom Assessment Scale (ESAS) with 0=no symptom and 10=worst possible symptom and quality of life using the Functional Assessment of Cancer Treatment: Leukemia (FACT-LEU).
Results: Participants had a median age of 71 years ( range:61-88y); 50% were female, and 87% white. Frailty Index results for 76 patients were 28 (36.4%) fit, 25 (32.5%) intermediate, and 23 (29.9%) frail. (One patient did not complete the mGA). 52 of 77 (69%) enrolled patients were alive at 3 months; 21(27%) died and 4 (5%) were lost to follow-up. Providers were asked the fit/frailty status prior to seeing the results of the mGA. Of 75 provider responses, results were 27 (36.0%) fit, 29 (38.7%) intermediate, and 19 (25.3%) frail. There was 63% (n=47) provider concordance with the mGA result. There was more agreement with fit (n=22, 81.5%) and frail status (n=11, 57.9%) and less with intermediate (n=14, 48.3%). Of the 25 of 75 (33.%) provider reports that indicated that the mGA result influenced the treatment decision, 6 patients (5 fit, 1 intermediate) received intensive treatment, 15 received non intensive treatment (1 fit, 6 intermediate, 8 frail) and 4 enrolled in a clinical trial (1 fit, 2 intermediate, and 1 frail). Significant symptom improvement at 3 months was seen for drowsiness, lack of appetite, shortness of breath, and anxiety. FACT Leu results did not change over 3 months. Providers reported an average of 4.45 minutes to review the dashboard. Patients were able to complete the surveys unassisted in an average time of 16.24 minutes.
Discussion: There was nearly 40% discordance between the provider and mGA, with the most discordance on the intermediate fit status. However, results of the mGA influenced treatment decision making in one third of provider/patient interactions. Further analysis of the mGA domains is warranted to see if additional insights can be gained. With time, some symptoms improve and others don't. This points to the opportunity to direct resources towards symptom assessment during treatment. Feasibility was demonstrated in this study as providers received the aggregated results in real time and reviewed them in less than 5 minutes. In addition, patients were able to complete the survey unassisted without disturbing clinic operations.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal